BTN.com staff, July 9, 2016

Alone, Anopheles gambiae, a species of mosquito native to sub-Saharan Africa, is a minor nuisance, but frequently it carries a malicious passenger: Plasmodium falciparum, the most dangerous strain of malaria to humans.
According to the CDC, there were an estimated 214 million cases of malaria worldwide in 2015. In that year, malaria claimed the lives of 438,000 people worldwide, many of whom were children in sub-Saharan Africa, one of the most active locations in the world for the disease.
To The Ohio State University biochemist Dr. Abraham Badu-Tawiah, that number is unacceptable.
?The problem in Africa is that people wait until they are sick to go to the hospital for a checkup,? explains Dr. Badu-Tawiah, who hails from Ghana. ?We want to bridge those that live in the remote areas to those that live in cities. The cities have most of the resources that are not available to those in the outskirts.?
Current means of diagnosing malaria call for testing a fresh blood sample, a procedure that necessitates arduous travel from those remote areas into cities to visit a hospital or clinic. Thus, most don?t chance the journey until the symptoms of malaria are upon them and their treatment options are limited.
Soon, though, that outmoded system may be a thing of the past, thanks to a groundbreaking innovation developed by Dr. Badu-Tawiah and his team at OSU that places the means of testing in the hands of those affected.
?The novelty of this work comes from the fact that we developed a new ionic probe,? says Dr. Badu-Tawiah. ?It is a simple organic compound that is stable to heat, stable to light, stable to dryness, stable to humidity, stable to anything at all.?
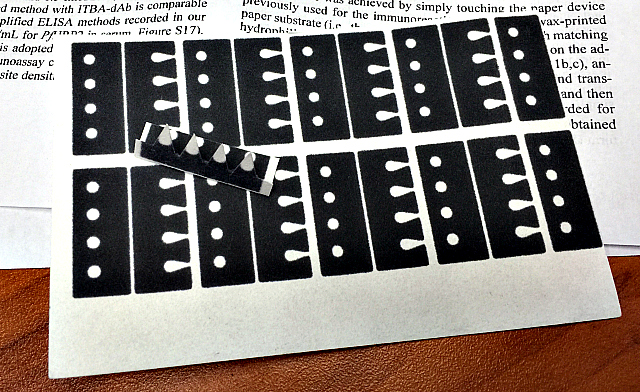
It is this stability that he hopes will save countless lives. In its current form, the test involves a small strip of paper, not much larger than a postage stamp, onto which an individual places a drop of blood. The hearty design, which has been shown to keep samples viable for up to a month, allows the patient to then mail the strip to the nearest facility equipped to analyze the test.
The small scale of the test strip is a crucial design component as it allows for health care providers to use smaller and, more importantly, cheaper handheld versions of the mass spectrometer needed to do the analysis.
?[People in] villages rely on towns for many things,? says Dr. Badu-Tawiah of the realities of rural African life. ?They grow crops out in the villages and then go to town to sell them. I?m hoping we could have one of these small mass spectrometers and put it in a small town center. When they go in to do their normal things, they can actually analyze for themselves.?
As for the immediate future, Dr. Badu-Tawiah is working to secure NIH grant funding to conduct large-scale testing in Africa of the procedure?s viability. His team is also working on making the strips more sensitive with the hope that urine or saliva could one day be analyzed the same as blood, allowing for easier and safer sampling for children and pregnant women.
By John Tolley
Photos: Pam Frost Gorder – The Ohio State University







